
PegaWorld | 43:43
PegaWorld iNspire 2023: Blue Cross Blue Shield Michigan & EY – Improving Customer Satisfaction via CMS Star Ratings
A key metric of customer satisfaction is defined by a health insurer’s star ratings, as determined by the Centers for Medicare & Medicaid Services (CMS). Blue Cross Blue Shield of Michigan (BCBSM), which provides health benefits to over 4.3 million members, was experiencing a decline in its star ratings due to operational and technical issues within its Grievances and Appeals process. With a potential impact of hundreds of millions of dollars in lost revenue, discover how BCBSM engaged EY to assess the situation and initiate an extensive remediation program to address the issues and improved their customer satisfaction star ratings.
Transcript:
- First of all, thank you guys for joining us this morning. I apologize, I know I, and probably my colleagues will be squinting through this entire presentation. So we're gonna do our best to stay on task and deliver hopefully what'll be valuable information for all of you this morning. Just by way of introduction of myself, my name is Amy Frenzel and I am the Executive Accountable at the Blue Cross Blue Shield of Michigan Plan for what we call Service Operations, which is typically what most plans will call customer service. And included in that is our Grievance and Appeals Processing Function and team. And we're here today to talk to you guys a little bit about the journey we went on with our partners at Ernst and Young regarding the work that we did to improve really our entire ecosystem, but a big portion of that being our Pega application to support our performance as it relates to our Medicare Advantage Stars ratings. So before I dig into the content, I'm gonna ask my colleagues to introduce themselves and then we'll get going.
- Hello everyone. My name is Monica McKinney. I'm actually the Director of Grievances and Appeals at Blue Cross Blue Shield of Michigan and Blue Care Network. It's a great journey and I hope you enjoy what we have to share.
- And my name's Tim Calhoun. I'm a managing director with our EY Health practice. I also have responsibility for health plan operations across the US. And most importantly, I've had the opportunity and privilege to work with both Amy and Monica and their teams along this grievance and appeals journey that we're gonna talk about tonight. So with that, I will second what Amy said. Raise your hands when you have questions at the end, and that way we can see it. 'cause right now you're all looking angelic.
- Yeah.
- Everyone has a halo, which is lovely. So, okay, well let's get going. I'm gonna start by just giving folks a little bit of background on our plan at Blue Cross Blue Shield of Michigan. We are the oldest and largest health insurer in the state of Michigan. We have about 4.7 million members and about 1 million of those members actually reside outside of the state. We are part of the Blue Cross Blue Shield Associations licensee program. So you probably all are familiar with the Blue Plan and whatever state you may come from, but we're here representing Michigan today. We also have a very large MA footprint for a Blue Plan. We have about 800,000 members in our Medicare Advantage product, and we are considered to be a high performing plan relative to Star's performance. And I'll talk just a little bit about Stars in a second to make sure everybody's got the context of what that program is, especially if you don't have familiarity with payers or with the Medicare Advantage Program. We have been a consistently high performing plan relative to Stars, but CMS, which is the Centers for Medicare and Medicaid Services, the government entity that facilitates the Medicare Advantage program, is making it increasingly difficult for payers like Blue Cross Blue Shield of Michigan to achieve that Star performance. And so our ability to maintain our high ratings in that program is critical for the success of our organization, for our customers, and for frankly, the beneficiaries of those programs who carry our health benefits. Let me take just a second to talk about CMS Stars program. So it is a system that measures the quality, performance and cost effectiveness of a Medicare health plan and also the healthcare providers on a scale of one to five. And so each year, plans who are engaged in a Medicare Advantage or the delivery of a Medicare Advantage program go through a very rigorous process of running the business day to day. And then we get ratings based on a number of different components that lead up to your overall stars rating, one star being the worst and five being the best. The ratings are published to the general public. So members who are shopping for health plan coverage for an upcoming enrollment year will go out to look at the ratings online and see that they probably would like to choose a high performing plan, four, four and a half or five stars. So again, it's critical for us for acquisition of our members and then retention of those members. They measure us in the Stars program on health outcomes. So how healthy are our beneficiaries, are our members who are carrying that Blue Cross card. They measure us on how well we run our plan operations and they measure us on generally just member satisfaction with their payer. The last thing I would want folks to understand, so hopefully this increases the compellingness of why we put so much effort on the work that we did in our G and A team. The stars measures include a lot of measures on things that are very subjective. So how did a member feel when they called customer service? There's also a lot at stake for things that are very black and white. Did you process grievance and appeals in a timely manner according to what the metric for CMS is. The subjective measures are worth a lot more than they used to be in the achievement of Star's performance. And those are incredibly difficult for large payers like Michigan to achieve because they are very subjective and there are a lot of things that influence them. So what that means for a payer like us is we really have to focus on the very black and white measures, perform at a five star level to the extent possible, almost near zero misses, so that we can keep those ratings up to offset the higher risk ratings where it's more difficult for us to achieve those. And in the end, if you hit certain star ratings, four, four and a half, five, there's a bonus payment that comes from CMS worth hundreds of millions of dollars to our plan. So it's also a big piece of our P and L, quite frankly, very important to us. All right, so let me transition here very quickly into kind of the business problem and what we did in our partnership with EY to really focus on improving our Stars performance. So a key requirement, as I said, is to have these high customer satisfaction ratings. And we really have, as a plan, a large plan, have struggled with things like member satisfaction because there are so many other things that influence how a member may feel about their health plan. Some of it might just be they don't like the benefit, but there's not really much we can do about that. If the group customer, for example, is purchasing those benefits, this is what they say that their employees are going to get. And so we really had to dig in quickly and with a lot of effort around where are the opportunities we can go to improve our performance on some of the other measures like grievance and appeals. And we did this in partnership with our friends from Ernst and Young, and it was really a journey over a few years, I think, when it was all said and done. And we really did focus on people, process and technology as we were looking at how we could improve our Star ratings in GNA and then make sure that that was gonna be reliable, consistent performance going forward. But the focus for today is to really talk about that core technology component. We use Pega as our GNA platform and we knew that there was going to be a lot of lift we would get if we really took a step back and thought about how do we optimize the investment we've made in Pega for supporting GNA processing. And we'll talk about the journey that we went through to do that. So I think, am I running maybe a slide behind here? No. Okay. So on this slide we had a G and A platform with Pega that we had put in probably a couple years before we started, two or three years before we started this kind of journey to revise and review it. And we were really, really seeing that we were having challenges quite frankly, with the platform. We weren't getting the kind of processing timelines that we wanted out of it. We needed to redesign our workflows. We had a lot of challenges with the system stability, quite frankly. And let me be clear, this was not a reflection on Pega as the platform. This was really a reflection of the work that was done to implement it initially and the approach that was taken, which, you know, frankly didn't quite follow what we would've called Pega best practices in terms of how we designed the program and engage the business to do the sprints and deliveries. And so as we identified that we need to do a lot of work here, we've partnered with EY coming out of an assessment of our current state. We're really talking about what would it take to get to a better state in this environment. And then we started the work from there. So I'm gonna talk a little bit, or I have talked a little bit about kind of the context there, but Tim is gonna come up and then share with you guys a little bit of a deeper dive as to the assessment approach and then what we discovered and then how we started our journey to really improve the things in that particular space. Tim.
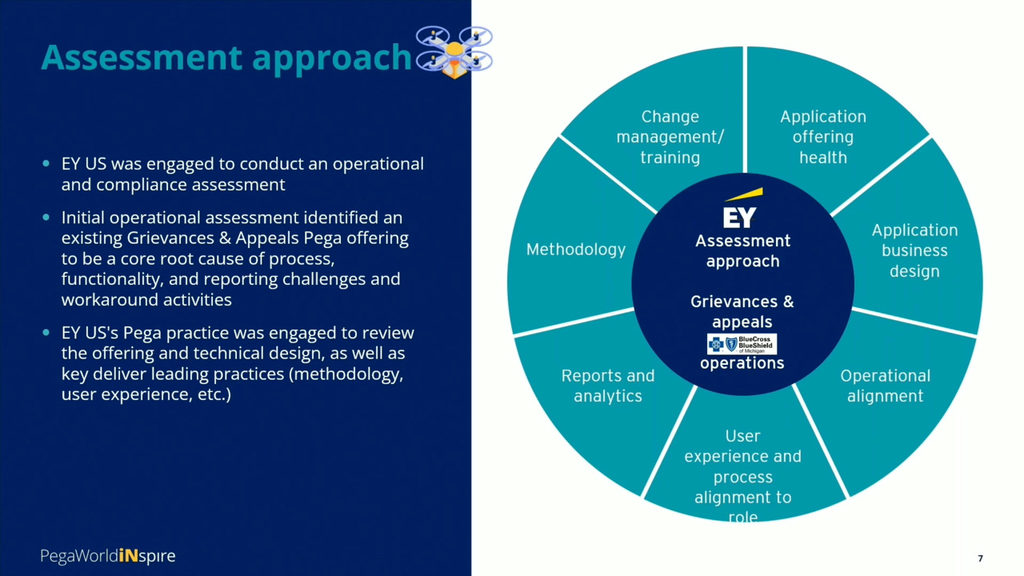
- Thanks Amy. I appreciate that. So every journey has a first step, and where we started was really around what was the problems and obviously Michigan was experiencing operational and platform challenges that were preventing their GA team to be able to address member and patient inquiries, but also the complaints on a timely and equitable basis. And this was deteriorating both member experience, but also Michigan team member job satisfaction. So based on our relationship and previous successes that we've had with Michigan, Michigan asked us to jointly come in with them and to take a hard look at the processes, the org alignment and the functional capabilities against what they would wanted to view as industry leading practices. And that joint team, that joint Michigan and EY team evaluated the pain points by reaching out to the grievance and appeals coordinators seeking to identify where areas of pain and conflict was existing, trying to further drill down into an established cause and effect relationships. Our initial focus was on process, a little bit of compliance and how coordinators, supervisors, and management was monitoring and responding to backlogs, bottlenecks and the actions that were being taken to resolve. We focused initially our assessment on four key areas. One was around the user experience, including the process alignment to profiles and roles, but also the processes necessary to support the regulatory compliance in internal and external SLAs. We also took a look at the operational alignment of the program and we also took a look and examined the reports and the analytical capabilities of the current platform. And also that led us into some change management and training discussions as well. As our assessment was identifying opportunities to streamline and improve operational functionality, we also began to suspect the challenges were beyond just process workflow and organizational alignment, but also the need to take a deeper look into the core Pega GA module as well as the core Pega platform. And at that point we decided to make an expansion of our initial assessment and we decided to pull in the our EY Pega practice SMRs to help take a look at that. And I'd be remiss if I didn't call out Ali Manshouri and Kate Griggs who helped us go through that effort and that review. Ali and Kate actually sat down and took a look at the information we had already captured and created, and then started to explore where potential implications were happening at the Pega and at core level, but also at the application level. We also then decided that it was that point in time where we needed to examine and extend the assessment into other key areas, the health of the application itself, the application of business design, but also the methodology that was being used to manage and maintain the platform, the application and the backlog inventory. The assessment identified the following needs: The requirement to revise and refine processes that were built as workarounds due to the fact that the GA coordinators were unable to complete a task or complete the case. Process refinement and re-engineering it in order to accommodate plan regulatory changes that were upcoming. And the need to provide critical workflow and bottleneck information for quicker decision making by coordinators, supervisors, and the management team. And of course, platform changes that were necessary to bring the full functionality of not only the application, but the full functionality Pega itself. All this was being done with the most importantly by looking towards improving member, patient and team member experience and satisfaction. What that I wanna bring up Monica to have her walk you through not only the journey that we took to rectify this, but also some of the outcomes and benefits as a result of that. Monica.
- Excuse me. Thanks Tim. All right. So when we talk about everything that needed to be done from refactoring, to building out the system and leveraging Pega capabilities, there were two things that stood out. The first that our guardrail score of 32 clearly indicated that there was significant instability with our tool. And then two, with all of the workarounds that have been developed to make the system work for us, it was clear that we were not using enough out of the box capability, and those that we were using, we weren't using as intended. It was also clear, as Tim stated, that in order to make all of this work, a true business product owner was needed to support the long term oversight and agile execution plan for the tool. And critical change management functions needed to be executed around organizational alignment, communication, and training. When we looked at the guardrail and refactoring, we took an immediate action to clear all of the warnings, we had thousands, make some critical corrections to the layer cake, activate what we considered to be non-used or dormant out of the box capabilities. We had to dismantle all of the workarounds and then build out a completely new end-to-end workflow process. The EY team led the charge on refactoring and rebuilding. They also helped us automate some of our testing and ultimately we were able to improve the guardrail score. As updates were released through our Agile implementation, feedback from our stakeholders was highly favorable and we measured that through quarterly satisfaction surveys. One of the really great outcomes as the updates were released was that our stakeholders told us that they had higher reliability in the system. And the high reliability was due to the fact that no longer did they have delays when they were actually trying to use the tool. And they actually didn't run into instances of lost or broken cases, which was a major pain point for us. While the IT teams were focused on correcting the infrastructure, EY continued to work with us to define the long term plan and roadmap. The results, and I'm very happy to talk about this part because I think sometimes when you have engagements, you don't always get a tangible, real roadmap, right? When the contractors go away, when the consultants go away, you don't have something that really sets the plan for the path forward, but we did. We walked away with a highly tangible, clear, prioritized approach to getting to best in class performance. It was designed to drive success through our Pega build, the known versioning capabilities and the appropriate utilization of the tool. We also saw increased satisfaction and engagement, particularly with our grievance coordinators and our nurses. They, along with members of our MD staff, actually started to use the Pulse capability, which allowed us to retain all of the case communication within one place. Prior to that, we were using emails and making phone calls and doing everything outside of the system, but using the Pulse capability allowed us to keep all of that communication within the scope of the case work. The other thing, excuse me, that needed to happen, and we knew that none of this would be sustainable if we didn't, make sure two things: One, that the business was very educated on the what's and hows related to how Pega works, how the Agile system works and how to communicate with the IT team. And we had to make sure that the IT team understood the business. Those two things were critical to making sure that we could effectively drive this forward. And so EY led the charge again, making sure that our G and A team, now with a new product owner and a new leadership team, 2.0, they took us through all of the Agile learning. They took us through all of the Pega learning. Each team came to the table fully engaged, that was a critical part of this. And we were able to drive optimal outcomes through the project with everybody there, making sure that we understood what the other was doing. And then also through this process, we built out more robust reporting within the Pega tool, enabling greater insight into ongoing monitoring of the stability of the system. We got greater insight into day-to-day operations. We were able to provide some really robust overall analytics, not just for us, but also for our stakeholders. And we were able to provide our executive leadership with that cross-functional view of what was occurring in our environment. So I know you guys are all sitting here wondering what happened? How did we do? What were the results? And I'm happy to say that 2022 was a banner year for us. We worked really hard and one of the very first things that we accomplished was a reduction in our turnaround times by 10 days. And that was huge for us out of the gate. That brought us closer to our SLA adherence targets. And then we also, by doing that favorably impacted our Star rating performance outcomes, bringing our score within hundredths of the five star threshold. We were most proud of that. Thank you. Very, very proud of that. In addition to that, you heard us talk about the guardrail score being at 32. By the time we ended our engagement with EY, our score was at 95 and we've maintained it in that area. I think currently we're at 92 and that just has to do with some things that were not out of the box that we had to implement since then. Our new end-to-end process helps us identify and move the work to the first available coordinator. This was huge for us because prior to that, we would have work sitting in individual work baskets and that meant that whomever had it may not be the first available person to work on it, right? So we were experiencing late or expired cases as a result of cases sitting, waiting for someone to come and work on them, we're now able to move that work to the first available person. And by doing that, we were also able to reduce the volume of expired cases in 2022 by 75%. Huge. You also heard me state that higher reliability was an outcome. And the key thing there was that that higher reliability drove greater confidence in the Pega tool, which helped increase the rate of adoption and the capability utilization across all of our stakeholder groups. We're still working with our MDs, they're a little slower, but all of our GCs, our grievance coordinators, all of our nurses are fully utilizing Pega at this point. The automation and testing and key process points enable the IT work to move faster with greater implementation accuracy. Utilization of the post tool continues to support capacity optimization by again, keeping all of that documentation and communication in one place and attached to the casework. Our reporting enhancements coupled with the API work that was completed enabled us to enhance our reports, our expert, all reporting. And we were able to again, create those executive KPIs and dashboards. We were able to drive and deliver increased analytics and insights, all of which remain and are growing in demand across our existing and even new stakeholders that have an interest in what's happening in the GNA space. Additionally, these reports really helped us sunset some highly manual and duplicative processes. Because we were able to establish daily operational reporting that gave us key insights. We were also able to eliminate a lot of our email processes and that saved us in 2022 from sending over 7,700 emails. Huge. We got all that capacity back. So the question I'm sure you're asking is, do we still have some challenges to overcome? Absolutely. It's GNA, and for those of you who know what this life is like, we're always chasing a moving finish line, right? But ultimately the good news from this engagement, from the use of the Pega tool is that our enhanced reporting supports a comprehensive and early understanding of our challenges. Our collectively developed roadmap, which I can't say enough about, I promise, serves as our blueprint for the future and we are leaps and bounds ahead of where we were two and a half years ago. And we are continued to be focused on, highly focused on continuous improvement. So very, very happy with that engagement. So at this time, I think I'm gonna open it up for questions. Anybody have questions for us?
- [Donna] I do. I have one. Hi, my name is Donna Brown. How did you get buy-in from all of the coordinators and everything from using different systems and getting that buy-in that process for a hundred percent. 'Cause people get stuck in their ways and how did you go about getting that buy-in?
- So it started, I'm gonna take it. Okay. It really started with a full understanding of the scope of change management that had to occur. We started off, and I say we, I came in probably in March of '21 with an understanding of we need to make sure that people understand the why behind the what we're doing. And we started with that. We've held town halls every quarter. I hold monthly meetings with my entire staff because I wanted them to understand the roadmap as much as I did. I wanted them to have a vested interest in what happened next. So we did those satisfaction surveys every quarter. We met with them once a month. We had bigger meetings quarterly to make sure that they understood what the direction was, the why behind it, and that they had an opportunity to really share their pain points so that we could continue to incorporate those into our Agile updates and implementations. So that was the key, was the communication.
- I think I would also add, and I think Monica would agree, our experience using Pega in our plan is really that it is about the end user. And so we really try to involve the folks who are gonna be using the platform in the development, the build and the roll-outs of the various sprints. And so I think there was a lot of what's in it for them as the end user and the more you engage, the better your day is going to be, quite frankly, because we needed them to be effective in the role. And then kind of peripheral to this, because of the importance of Stars, we really spent a lot of time focusing on recognizing that team for what they are delivering. I mean, when I say there are hundreds of millions of dollars at stake, that is not an exaggeration. And the performance of this team is a big part of our ability to achieve that. And so I think the attention that we were giving them and the recognition and the appreciation for what they do and how they were engaging in this process was also a critical piece.
- Yeah.
- I think one other thing that I thought was very successful is they were actually involved in the prioritization and the trade-offs of each sprint at each release. They understood, they gained a perspective of that Agile approach of understanding story points and making trade-offs that are equal value, equal duration and understand that, you know, something may get pushed back, but it's not necessarily gonna be totally forgotten. That backlog inventory was kept in front of them and communicated as to when it was gonna happen.
- Question here guys. How else are you using Pega at Michigan? Do you have other applications besides the A and G application? And then what kind of support for those applications or for the D and A application you have as far as developers, product owners, business owners, how does that group make up? And then what comes next? Talk about the roadmap you have. Where do you go with this?
- You've got like three questions. Do you wanna?
- So I'll start and then keep us honest if we forget one. So we at the Michigan plan, not only use Pega for all of our GNA work, both on the MA side and on our commercial business, we also use Pega CDH for our contact centers. And so full transparency, I think my partners from NASCO entered the room not too long ago. NASCO is a subsidiary of Blue Cross Blue Shield of Michigan and we actually work with NASCO. They deliver our Pega products to us as a plan. And so part of the structure for support as we were getting started prior to these being NASCO delivered products, we would work with consultants and partners like EY and others to do our original implementations. And then now we partner with resources at NASCO, primarily on the technical side I would say. And then we've got folks like Monica as a product owner. There's a gentleman on my team for the contact center side, and then Lori I think is in here somewhere. We've got certified Pega folks in the business. And I think this is, I would just point out to folks in the room, I'm not sure if everybody's using Pega, you're contemplating Pega, but along the lines also of the change management. The use of Pega at our organization was very transformational. We are a dinosaur, ginormous, very old school, legacy, waterfall approach to everything. And to be successful, I think working with Pega, you really need to invest the time to help the organization and the key players, stakeholders understand that it is a totally different model. It is business driven, it is not necessarily IT driven, the ability to help people understand their involvement in defining what the capabilities are, the KPIs that they're tied to, the whole entire process of developing stories and sprints and the constant deployment. There are quick returns with Pega in terms of, we used to do one release a year and so our backlog just grew and grew and grew and grew and people got more and more frustrated and we would add work around after work around, making everybody's lives more challenging. In this model it is, you know, every other month we're doing releases of very impactful capability deployments. So we're in on Pega and my partner's from NANSCO over there in the corner, if folks have questions in terms of how we've done that delivery at Michigan, I'm sure they'd be also happy to talk to you as well.
- [Audience Member] So in your transformation, did you use process mining or any of these new improvements there that Pega's offering? Or is that something that you're looking to for the future?
- We are looking for the future, I think for the most part. We had some work to do to, well get that's the platform stable first. We've gone through an upgrade and we very much have our eye on what's next in terms of the capabilities, especially things that were talked about in the keynotes yesterday. One of the challenges we have quite frankly right now is we have a staffing issue. Our volumes are up 30% higher than what we forecasted and we're struggling to find talent. And so we are all in on anything that can be automated. Anything that can drive efficiency to help us find capacity. I can say without a doubt, had we not done this work with our partners at EY and put the time and investment behind this, we would be dead in the water right now because we would not have been able to take on a 30% increase and maintain our performance. Not to say it's been easy, but I'm so grateful that we got this work done when we did.
- Thanks. You mentioned that about a fifth of your membership resides out of the state, so that would presumably challenge your GNA operations a lot more. Did that have an impact on the assessment as well as the solution?
- It really doesn't. In terms of where our members are, there are nuances if you're a Blue Plan on what you can and can't do with how you engage with your members. And actually it's more the providers, our doctors and the hospitals, facilities. But for us, a member is a member and they carry a Blue Cross Blue Shield of Michigan ID card, and so everything is really, I would say, uniform in terms of the processes and how we engage with 'em relative to GNA, regardless of where they live.
- [Audience Member] Hey, so I was curious about a couple of points here, right? So the first one was, I was just curious, how did your time and motion effort, like whether y'all have done a time motion study and how did that a process to, I mean, the time to process an appeal of grievance, how did y'all see that improve? I know it could last over days, but if y'all did do it like, you know, in one go, how was the improvement there if y'all have done something similar to that. And about the process and usability corrections, right. I was just curious about what y'all did or if you could shed some light on what was done in that aspect.
- I don't think I heard all the questions.
- So on the SLA component, the improvement of cycle time, 10 days. We measured it from the moment the case entered into the system till the case had an ultimate resolution to it. And that turnaround time was how we measured the conclusion of the case and thereby was able to come up and identify that, you know, we were able to take 10 days out of the typical cycle that was being experienced during current state, and we continue to monitor that. It's set up so that monitoring can continue to go forward today. The last part of the question was around the technical refactoring. Was that correct?
- Usability.
- Usability corrections.
- So tell me, when you say usability, I think this is gonna be one of your answers, but tell me, when you say usability correction, what do you mean exactly?
- [Audience Member] Actually, I was asking the question about what y'all meant by that because it's on the slide.
- So a lot of the way we were using it was inefficient, right? We had people using duplicative tools. Because of the way the workarounds have been developed, they had to leave the system to go out and do things. When we worked with EY, we actually put that new end-to-end process in place and it was very different from what everybody customarily knows for GNA. And I'll just give you a little insight, GNA normally is done by one person. The case comes in, one person works that case, beginning to end. That is not our process anymore. Because of the volume, we needed a workflow that allowed that case to move through to the first available person at every cycle. So putting that in increased the way in which we were able to send the cases through the workflow. It increased the speed with which we were able to send the cases through the workflow, it increased the pace with which we were able to mobilize people to the casework and then ultimately increase adoption of the capabilities. So when we're talking about usability, it was just throughout that end-to-end process, we stopped having to toggle out of the system. We stopped having to use multiple resources to support us. We were able to contain, I guess the process within the Pega tool.
- I would also put in that bucket, the refactoring that was done. I mean, the coordinators quite frankly would be staring at clocking.
- Yeah.
- Like the system would become latent, they would get kicked out of the system, cases would go missing. Parts of cases would go missing.
- Yeah.
- So there's a lot probably in that usability bucket that came through both the refactoring process to improve the stability of the system and then as we did the go forward different capability deployments. But there's a lot I think in usability because again, it was really built by the coordinator staff to make their usability of the system better.
- Hey, good morning, we at Blue Shield, we are doing a pilot of Pega, you know, for appeals and grievances, primarily for the nonclinical appeals. So we would want to extend it at a later time once this is successful. So as you have done it at your end, so did you see some significant improvement as far as the business operations are concerned, especially around SLAs or case turnaround times and any of the cost benefits you might have seen? Right. So because before going, we have seen a lot of value proposition for us. But as you have already done it, like, you know, do you want us talk about it?
- Yeah, we saw, that turnaround time was an average across all case types. We were actually able to considerably improve, especially for appeals, because for those of you who know, that is what Stars is measuring. So we focused on being able to prioritize the case work and carving out those days and continuing to kinda sustain that performance is key. And I think I'm missing the second part of your question. Say the second part.
- No, yeah, I mean some of the cost benefits you might have realized, you know.
- Oh my gosh, like just, I'm gonna tell you guys just the sheer fact that we've been able to build in this capacity, it's hard for us to, and when I say this, it's kinda like six in one hand, half dozen in the other, right? If the work stayed stagnant, we probably would've reduced our need for staffing by at least 10 people in this process alone. And I know that's a very high claim to make, but I believe that to be true just in the capacity of carving out and eliminating emails, right? But because our volume increased, we didn't necessarily see it, but we know it's there because as Amy stated, had we not done what we did, we would be so far off the mark right now from where we need to be.
- We would be having to hire exponentially
- Yeah.
- In the old model compared to what we're requiring for staff now.
- Yeah, yeah. So from a cost benefit standpoint, you know, it's just that driving that change in the capacity, the utilization of how the staff is accessing the work. All of that hands down was, I wish I had a number for you. I don't, I'm just telling you, it was bodies.
- [Host] We have a question here and then they'll let you.
- So assuming that you are currently in the latest maybe Constellation, how challenge, oh, can you hear me now?
- Yes.
- So assuming that you are currently using the latest Constellation or even theme Cosmos, right? How challenging was it to kind of integrate with all the legacy systems, which we all have in our, you know, company.
- So for us, and Tim, you may know more from an IT standpoint or even Krishna. We try to streamline the process to make it really easy to ingest casework, right? Casework comes in through fax, casework comes in through mail. We do get some from our customer service team. So we allow customer service to enter right into Pega. That solved that problem right away. The next problem was how do we get the faxes and the emails in? And we were able to connect our fax box and our email box, I guess one and the same really, to Pega, I'm gonna say very easily. That's probably an exaggeration, but very easily. Like that was not a concern for us at the time. We don't have necessarily all of, oh, and let me back up. Because we were using a different membership tool. So we did have to do some work to ingest that data into Pega and we are actually retooling that now because we're implementing that on a Pega platform as well. So once that happens, it will be seamless again. But I don't believe that of all the things we implemented, integrating to the tools that needed to help feed information into our system was difficult.
- The only thing I'll add is part of the design sessions that we had was to lay out, you know, where was this data coming from? For those of you who have Pega today or are using Pega today or in the midst of an implementation, you know that Pega comes with a great deal of API capabilities. It allows it ingest that data. The trick though to that was understanding where that data existed today so that we could plan accordingly to build the integrations into the Pega platform if it didn't already exist. So those are the type of things that you really should be aware of as you're going through your design sessions, is not only just design the process, but where does that data come from and laying that out. So I think that's probably a little bit of the trick or the spice to the sauce as it were. We got time probably for one more question. Anything else? Alright. Oh, okay. Thanks Ali.
- [Audience Member] First of all, thank you for a wonderful presentation and having your patience for answering all of our questions. So I saw one of the solution approach that you took was corrections to the layered cake, right? So you already have users in place and workflow process in place. How did you manage to, in the interim, how did you manage to handle the in-flight traffic while you implement the new approach? Did you face any challenges in handling the ongoing in-flight traffic?
- I wanna say that the EY team worked very closely with our IT team to really insulate us from that. They built out the corrections in the dev environment first. We were able to do a lot of the testing there before they moved it into production. So the staff, you know, we didn't get any post, I shouldn't say any, but we didn't get a lot of post-implementation issues. I mean, in fact, we had very few while they were working on that because they did everything in the dev environment first. And I know Krishna's sitting here, he's kind of shaking his head at me, so.
Recurso relacionado
Producto
El diseño de aplicaciones, revolucionadoOptimice el diseño del flujo de trabajo, rápidamente, con el poder de Pega GenAI Blueprint™. Configure su visión y vea cómo se genera su flujo de trabajo en el acto.
