
Pega Smart Claims Management for Healthcare
"Since going live with Pega's smart claims engine functionality last year, we've had a number of solid wins. We have created a powerful modernized foundation and ... we have started to radically re-engineer claims processing; and have a path and a plan to achieve end-to-end claims automation that is real, today."
Get to know Pega Smart Claims Management
Eliminate gaps with
targeted claims processing
targeted claims processing
With Pega’s robust business rules capability and healthcare claims models, you can easily configure claims processing business rules that legacy systems can’t support, including pre- and post-adjudication rules, to improve auto-adjudication rates.

Manage change with
configurable workflows
configurable workflows
Adapt swiftly to evolving government regulations and the needs of your business with Pega’s configurable workflows. Utilizing intuitive, business-friendly modeling tools, users can easily establish optimized claims processing workflows or tailor pre-defined components to their needs.

Make every claims examiner
an expert
an expert
Improve efficiency and accuracy across your Claims Examiner staff by making every examiner an expert. Pega’s embedded claim resolution guidance, with AI-ready intelligent workflow automation, supports claims examiners through pend investigation to the correct resolution.

Transform claims process management with
AI-powered automation
AI-powered automation
Leverage Pega Smart Claims Engine – with its advanced AI capabilities – to reduce cycle times by up to 80% while maximizing straight-through processing. The system continuously learns and adapts, leveraging GenAI for intelligent document processing, Process AI for dynamic workflow optimization, and Agentic AI for autonomous and/or augmented decisioning.
Adapt and comply with
on premise or on cloud
on premise or on cloud
With Pega, you can develop a claims processing capability that reflects your business while supporting HIPAA compliance. Choose traditional on-premise deployments or Pega’s cloud platform, which features a turnkey service providing immediate access to create, test, deploy, and manage applications.
Additional Product Features
Rapid Implementation Boosts ROI
Included best-practice workflows, interfaces, rules, data models and more jumpstart implementation.
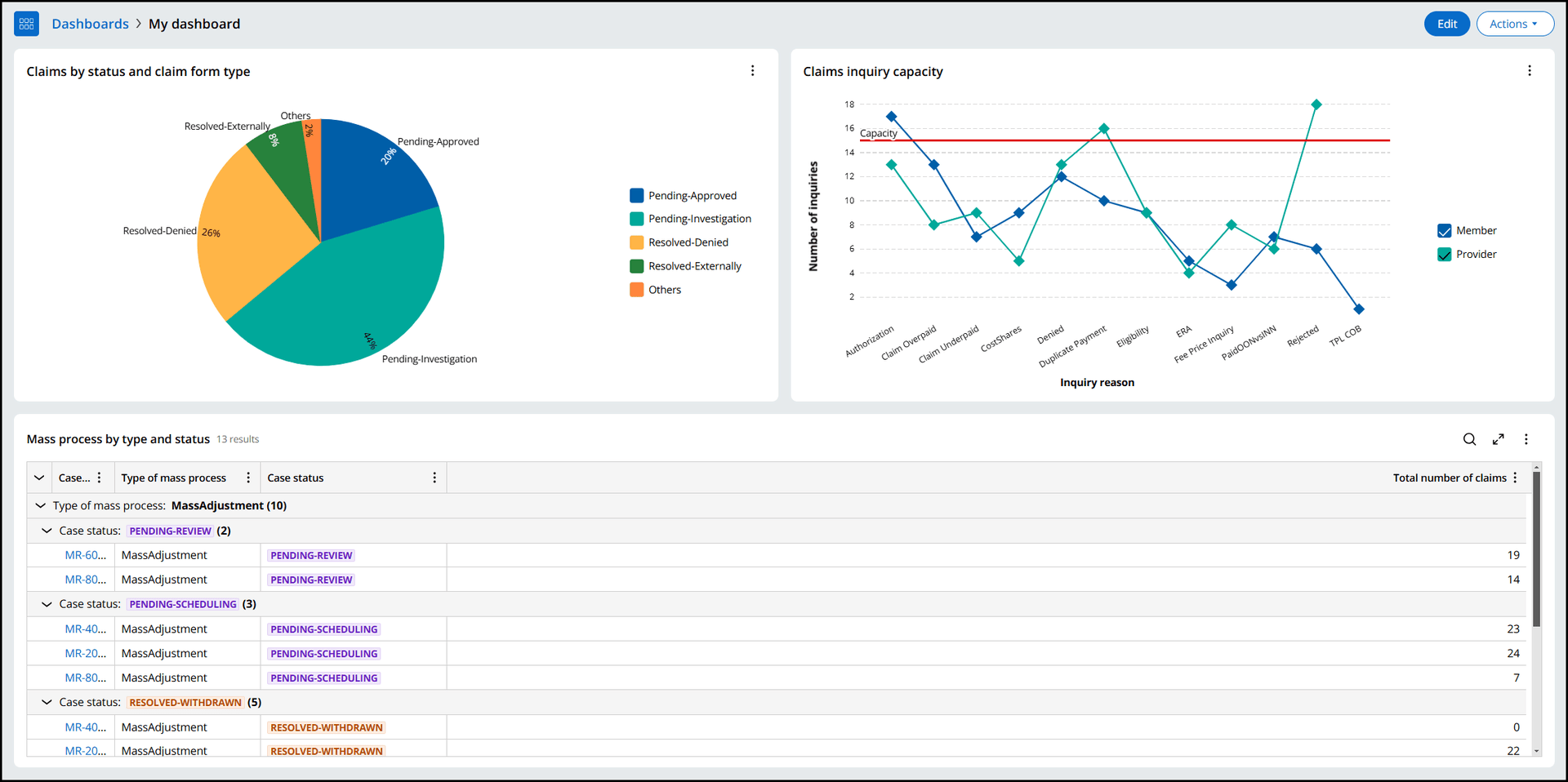
Intuitive and Actionable Insights
Accessible and engaging chart-based or comprehensive table-based displays so you can collect, customize, and share business intelligence across your organization.
Respond to Changes in Inventory
Dynamic claims inventory management enables you to easily direct claims for the most efficient and effective outcomes.
Make every examiner an expert
Easily create custom, dynamic pend resolution guidance to promote accurate and efficient pended claim resolution.
Speed Time to Market for New Products
Configure processing "outside the box" of legacy systems to rapidly implement products and benefits.
Consistency and Traceability
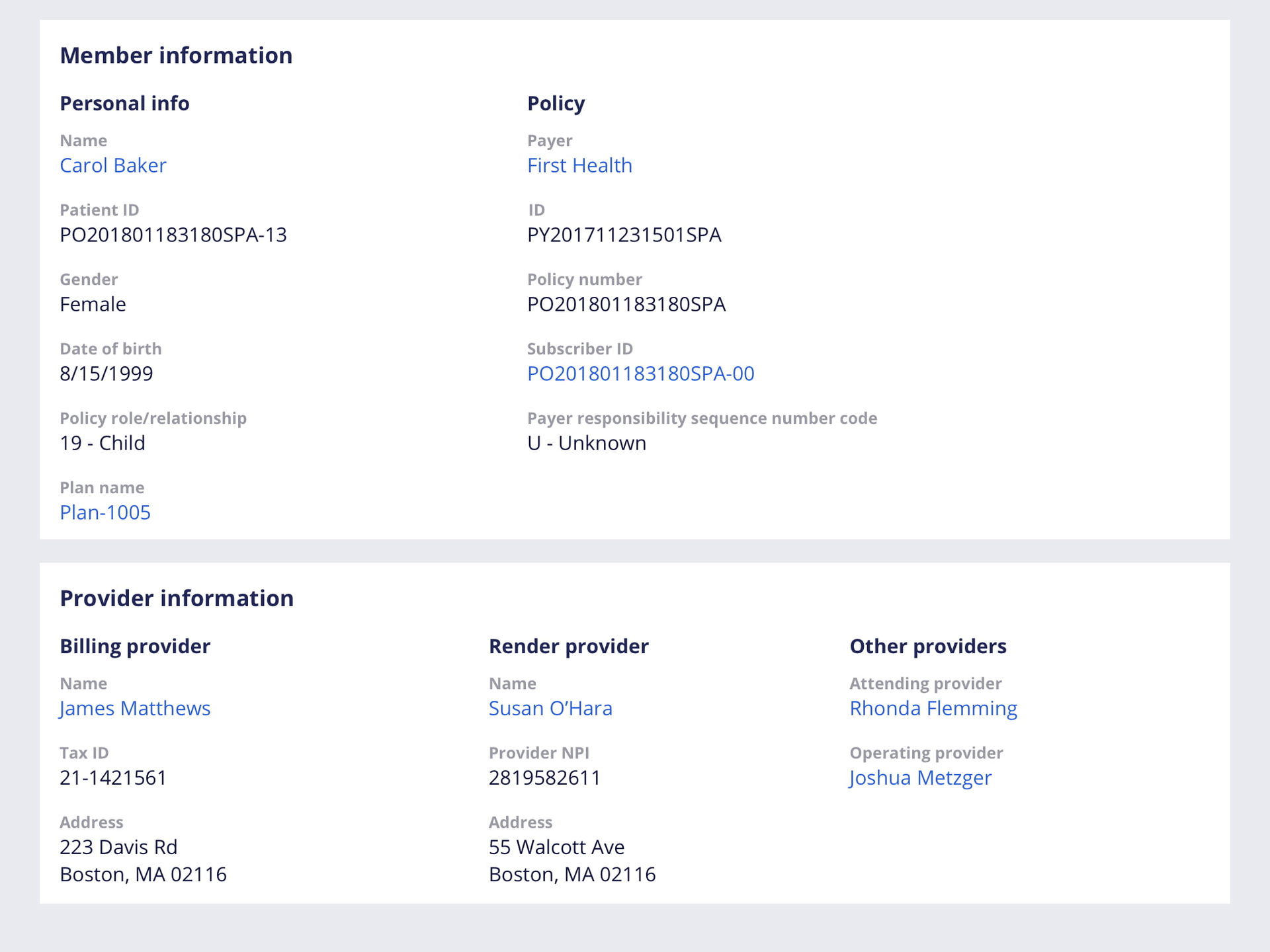
Automated tracking of system and user activities to ensure consistent, accurate, and timely response to members and providers.
